NAD+ has many important effects on health, including the anti-aging activity of enzymes that stimulate sirtuins and repair damaged DNA.
NAD+ is necessary for healthy metabolism and mitochondria. In addition, low NAD+ is associated with fatigue and several diseases.
Read this article to learn more about NAD+ and the factors that increase or decrease NAD+.
What is NAD+?
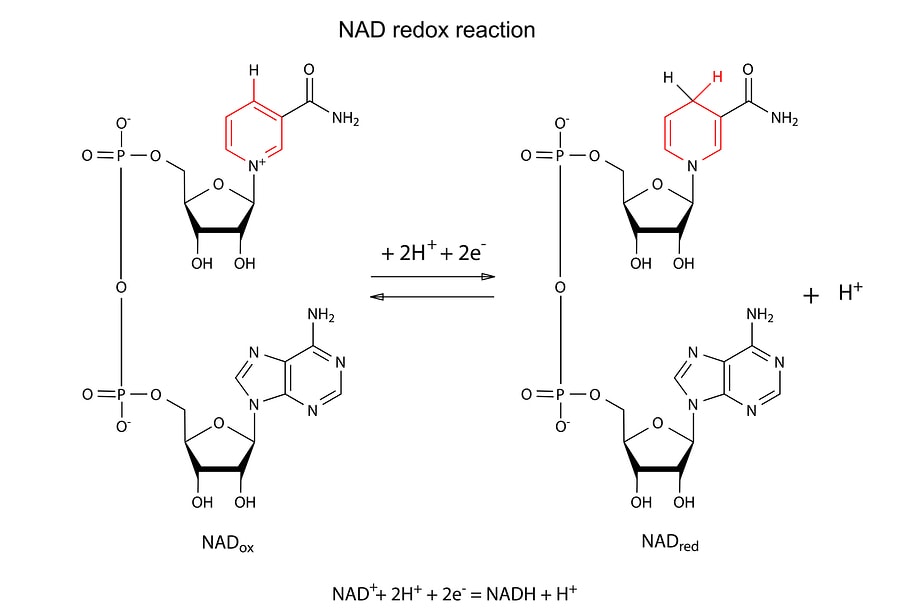
Nicotinamide adenine dinucleotide (NAD), a coenzyme composed of adenine and nicotinamide, is present in all living cells.
It exists in two forms: NAD+ and NADH; The main difference between the two forms is that NADH contains two more electrons than NAD+.
Genetic variations in genes that interact with NAD affect how the body processes this important molecule.
How is NAD+ produced naturally by the body
Electron transport chains in mitochondria
This 2-minute video shows the process of oxidative phosphorylation, which converts NADH into NAD+, producing three ATP molecules for every NADH used.
When our cells break down carbohydrates and fats for energy, the energy is stored by producing ATP and NADH.
The energy stored in the NADH electrons can be converted into ATP through a process in the mitochondria called “oxidative phosphorylation” or “cellular respiration.”
In situations where food is plentiful, or when our bodies break down (” metabolize “) more carbohydrates and fats, NADH levels rise and NAD+ levels decrease.
When electrons pass through the electron chains of the mitochondria, energy is produced.
NADH is the most important carrier of these electrons, and when it releases them, it becomes NAD+. The body gets energy from food through the electrons in food.
When you have the ingredients to use those electrons, you tend to feel more energetic and healthy – and when you don’t have the proper input, you may feel weaker.
How is NAD+ produced?
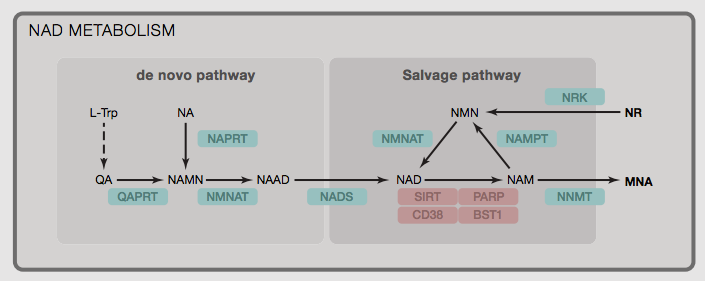
The following are the “raw materials” or “building blocks” (metabolic precursors) needed by the body to produce (synthesize) NAD+ :
- Nicotinamide ribose (NR)
- Tryptophan (L-Trp)
- Niacin (NA; Also known as vitamin B3)
- Niacinamide (NAM, also known as “flushless niacin”)
- Nicotinamide mononucleotide (NMN)
In general, supplementing NAD+ precursors involved in the “remedy pathway” (such as nicotinamide ribonucleoside and NMN) is relatively more effective in raising cellular NAD+ levels compared to precursors involved in the “de novo” pathway.
This is because the NAMPT enzyme can act as a major limiting factor (” bottleneck “) for NAD+ production.
However, not every cell will be able to convert each of these precursors at all times, as many of these precursors also have other important roles in the cell (and therefore cannot be fully used to make NAD+ alone).
The following biochemical transformations or pathways occur in these cells:
- Tryptophan enters NAD+ : liver, neurons, and immune cells
- Conversion of niacinamide to niacin: intestinal bacteria
- Niacin (B3) enters NAD+ : liver, kidney, heart, and intestinal cells
- Rescue methods: heart and skeletal muscle
NAMPT activity may be reduced by circadian dysregulation and inflammation and increased by exercise.
Supporting each of these pathways may increase NAD+ in these tissues or organs, but not others. The relative activity of these different pathways may also depend on other factors, such as stress levels, inflammation, and circadian synchronization.
11 potentially harmful effects of low NAD+
It is important to understand why low NAD+ is associated with health problems.
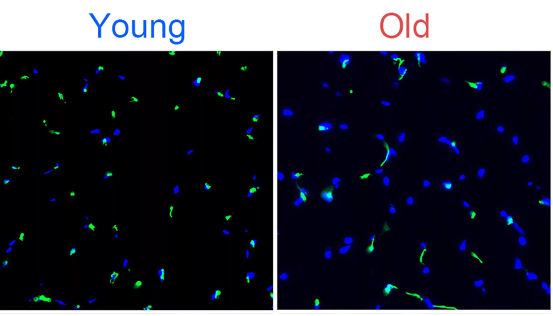
1) Aging
In the mitochondria of young people, NADH can easily supply electrons to produce NAD+. During aging, increased DNA damage reduces NAD+, leading to decreased SIRT1 activity and decreased mitochondrial function.
NAD+ levels decline with age and oxidative stress.
The more NAD+ levels increased, the more SIRT1 was active (niacinamide, on the other hand, blocked SIRT1 activity).
Low NAD+ reduces SIRT1 activity, and low SIRT1 activity is associated with aging.
In addition, a decline in the function of genes that control circadian rhythms during aging reduces NAD+ levels.
In turn, SIRT1 also plays a huge role in circadian rhythm gene expression, which again plays a huge role in all of our cells.
2) Hypoxia
When you’re deprived of oxygen, your mitochondria don’t work properly, and for good reason. Oxygen needs to be there to receive electrons from the mitochondria.
When you’re low on oxygen, it can’t accept electrons, so your body wants to slow down the function of your mitochondria.
When you are low on oxygen, your body responds by slowing the conversion of NADH to NAD+ (reducing oxidation). Therefore, the accumulation of NADH and the relative reduction of NAD+.
Low NAD+ is called “pseudohypoxia” because even if you have adequate oxygen levels, the body will have some of the same reactions to low NAD+ caused by low oxygen.
Low oxygen in the cell also causes an increase in NADH and a decrease in NAD+. Low NAD+ reduces SIRT1, which leads to a higher Hypoxia Inducible Factor.
3) Sunburn and skin damage
NAD+ and NADH protect you from skin damage/burning and skin cancer in the sun. NAD+ mainly absorbs UVB spectrum, NADH mainly absorbs UVA spectrum.
I suspect that people with low NAD+ levels tend to get sunburn very easily. This indicates low MSH and/or low NAD+.
4) Fatigue
Fatigue, low physical strength and mental capacity are also signs of low NAD+/SIRT1.
The level of NAD+ largely controls the “REDOX potential” because of the ability of NAD+ to acquire electrons.
The higher the REDOX potential of the cell, the better the mitochondria work, the better it can fight infection and perform the function that the cell is supposed to.
Supplementation with NADH, NAD+, or their cofactors can help treat chronic fatigue syndrome and fibromyalgia.
5) Weight gain and metabolic syndrome
NAD+ activates Sirtuins, apparently turning on genes that improve metabolism, help with weight loss and lower LDL cholesterol. In addition, niacin and other NAD+ precursors are being tested as treatments for cardiovascular disease.
In a mouse study, supplementation with nicotinamide ribose, a precursor of NAD+, prevented diet-induced obesity. These animals also burn fat better, burn more calories, and become more sensitive to insulin.
Sirtuins improve glucose levels and glucose homeostasis by increasing insulin levels.
Metabolic syndrome is closely related to depression. This low Sirtuin activity, combined with decreased NAD+ and reduced tryptophan availability due to inflammation, may worsen depression.
6) Cardiovascular disease
Mitochondria are heavily used by the heart muscle, and Sirt3 is required for mitochondrial activity.
NAD+ depletion, often caused by DNA damage in failing hearts, can accelerate heart failure in laboratory animals.
In cases of ischemia-reperfusion injury (damage to the heart due to insufficient blood flow), NAD+ levels also decrease.
Therefore, methods to increase NAD+ and activate Sirtuins have been proposed as a treatment or complementary treatment for heart disease.
7) Multiple Sclerosis (MS)
During chronic nervous system inflammation, the activation of Th1-derived cytokines by CD38, an enzyme that uses NAD+, can reduce the availability of NAD+ outside the cell.
In multiple sclerosis patients, NAD+ is increased in the immune system and decreased in the nervous system.
In multiple sclerosis patients, NAD+ is increased in the immune system, but neuronal NAD+ is lacking. In addition, patients with multiple sclerosis have less serum tryptophan available to produce more NAD+ within neurons.
NAD+ deficient neurons are more susceptible to degeneration like MS.
In animal models of multiple sclerosis, NAD+ levels in the central nervous system are elevated due to changes in the immune system.
Increasing NAD+ by supplementing with NAD+ precursors or fasting helped improve multiple sclerosis in animals, but giving tryptophan appeared to increase the number of lymphocytes, making multiple dementia worse.
8) Oxidative stress
NAD+ increases the activity of antioxidant enzyme SOD2 through Sirt3.
SOD2 is an important factor in reducing cellular oxidative stress.
9) Metabolism and thyroid hormones
NAD+ controls metabolism (as well as hormones like T3), and low levels of NAD+ and T3 can make you feel cold due to reduced metabolism. In frog cells, NAD+ increases free T3.
10) Brain function
The brain has a high demand for energy, so neurons contain a lot of mitochondria. Mitochondrial dysfunction also contributes to a number of mental health and neurodegenerative diseases.
NADH therapy improves cognitive function in patients with Alzheimer’s disease.
In mouse models of Alzheimer’s disease, increasing NAD+ by supplementing with nicotinamide ribose restored cognitive function by increasing PGC-1α levels.
NADH has been used to treat Parkinson’s disease because NADH may increase the bioavailability of levodopa, which is used to treat Parkinson’s disease.
In rats, NAD+, given through the nasal cavity, reduces damage to the brain from hypoxia.
This is also why many of my clients claim that using niacin/niacinamide works better in the short term: because it increases NAD+.
My clients often claim to be better at using amphetamines in the short term as well. Amphetamine depletes energy, ATP, and dopamine in certain parts of the brain (the rat striatum).
When rats were given niacinamide to increase NAD+ levels, the negative changes caused by amphetamine were reduced.
We found that lower levels of NAD+ reduce brain energy and dopamine, and people will start to need stimulants to stay in shape.
11) Immune function and inflammation
Patients often have chronic infections and inflammation that they can’t get rid of.
Increasing NAD+ in animal models reverses autoimmune disease in various ways, suggesting that low NAD+ is one of the causes of immune system disorders and why autoimmune conditions often co-exist with chronic fatigue and brain fog.
NAD+ reverses autoimmune diseases by increasing anti-inflammatory Th1 and Th17 cells (which are usually bad, but NAD+ alters them to increase TGF-b and IL-10).
What we’ve seen is that we can make generalizations about the immune system, but subtleties are often crucial. Thus, NAD+ levels can turn Th1 advantage from bad to good.
SIRT1/NAD+ is important for the immune system to clear pathogens in part through MHC II activation. Hypoxia or low oxygen prevents MHC II activation by reducing SIRT1 activity (oxidized LDL also reduces SIRT1 in macrophages).
NAMPT that produces NAD+ also increases MHC II activation. However, by activating other Sirtuins, it can reduce pro-inflammatory cytokines and regulate the immune system.
NAD+ (along with SIRT1) appears to be one of the molecules that create the best balanced environment for the immune system to fight infection while suppressing inflammation.
Factors that may increase NAD+
Factors that make mitochondria more efficient and activate sirtuins typically increase NAD+, including fasting, caloric restriction, and ketosis.
Much of this research is early, speculative or of relatively low quality, so be sure to talk to your doctor about any changes you’d like to make to your diet, exercise style or supplements.
Factors that increase NAD+
1) Exercise
Energy stress from exercise causes cells to burn NADH for energy, which in turn produces more NAD+. NAMPT levels also increased with exercise.
Interval training is the most efficient way to create energy stress time. Aerobic exercise is another method that can provide the benefits of sustained energy stress over a longer period of time.
2) Diet
The ratio of NAD+ to NADH perceived by the body; If NAD+ is low relative to NADH, this is a signal of excess energy or too little oxygen.
High NAD+ levels may mean that the body has been using up energy and has a negative energy balance; That is, it burns more calories than it takes in.
When cells have more carbohydrates to burn, this leads to a buildup of NADH. The consumption of carbohydrates and nutrients causes NADH to be depleted, thus forming NAD+.
Fasting and caloric restriction (the scientific term for calorie counting and portion control) lead to higher NAD+ and sirtuin activation.
3) Ketosis/beta-hydroxybutyric acid
Fat-burning states, such as ketosis, increase NAD+.
A ketogenic diet can help you get into this state without having to fast.
4) Fermented foods and kombucha
Fermented foods and drinks, such as kombucha, contain NAD+, which is one of the reasons it gives me energy. Fermentation uses NADH to produce lactic acid, with NAD+ as a byproduct.
5) Sauna and heat shock
Saunas are also considered a panacea and have been a part of every historical culture. We think it’s because we’re expelling toxins, which may have something to do with it, but saunas and heat shock also increase NAD+ levels.
Since infrared also increases SIRT1, infrared saunas are ideal.
6) Fructose
Fructose increases the function of sirt1 and activates the mitochondrial enzyme that converts NADH to NAD+.
Honey and fruit are natural sources of fructose. We do not recommend consuming fructose alone because it may increase inflammation and promote weight gain.
Supplements associated with increased NAD+
These supplements have been linked to an increase in NAD+ in at least one human trial, but none have been approved by the FDA for this or any other medical purpose.
- Nicotinic riboside
- Malic acid
- Resveratrol
- apigenin
- leucine
- Nicotinamide – Low dose
- Lithium inhibits mir-34a
- Succinic acid
NAD+ intermediates
Supplementation of NAD+ intermediates may increase NAD+ in cells and mitochondria. Again, note that none of these supplements are approved by the U.S. Food and Drug Administration for any medical purpose.
- Nicotinamide – Low dose
- Tryptophan and aspartic acid are the fuel for NAD+, but if you eat enough protein, we usually get enough dietary amino acids
- Nicotinamide ribose (NR)
- Nicotinamide mononucleotide (NMN)
Although NR and NMN have been shown to reduce markers of aging in animal models, their efficacy in humans needs to be further tested.
Activating AMPK increases NAD+
AMPK increases SIRT1 activity (increasing NAMPT) by increasing cellular NAD+ levels.
SIRT1 activation also stimulates fatty acid oxidation and indirectly activates AMPK.
7 factors that reduce NAD+
1) Chronic inflammation
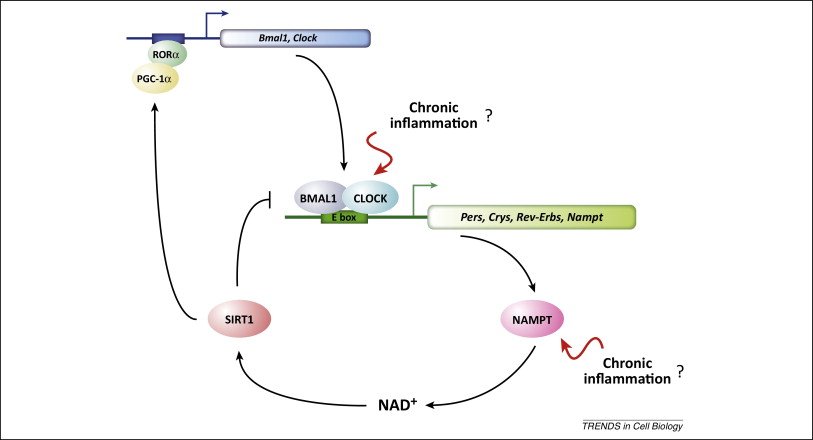
Chronic inflammation reduces NAD+ levels by inhibiting NAMPT enzymes and circadian rhythm genes.
2) Circadian rhythm disturbance
The circadian CLOCK genes BMAL1 and Clock control the production of the enzyme NAMPT, which is the final step in the production of NAD+.
The ups and downs in cell production due to circadian rhythms will lead to ups and downs in NAD+ levels. This ebb and flow decreases with age, which may explain why NAD+ declines with age.
Getting enough sleep each night is one of the best things you can do to improve your overall health and well-being.
3) Overeating
Low oxygen in the cell also causes an increase in NADH and a decrease in NAD+. Low NAD+ reduces SIRT1, which leads to higher hypoxia-inducing factors.
4) High blood sugar and insulin levels
High blood sugar levels lead to an increase in NADH and a decrease in NAD+. Insulin also increases the NADH/NAD+ ratio.
5) Alcohol
The chronic fatigue syndrome patients I coach do poorly with alcohol consumption because alcohol lowers NAD+.
Alcohol has many negative effects, but they don’t explain why people start feeling worse so quickly. NAD+ explains this almost immediate effect.
6) DNA damage (PARP activation)
A lot of DNA damage means that more PARP molecules will act on the damaged DNA and deplete NAD+. This decline in NAD+ can reduce the activity of Sirtuin.
7) Sirtuin activity decreased
Although NAD+ controls the activity of Sirtuin, low Sirtuin levels can reduce NAD+ levels in a number of ways, including:
Sirtuin controls circadian rhythms, so low levels of Sirtuin may disrupt the ups and downs of circadian rhythms, thereby reducing NAD+ levels.
Decreased Sirtuin activity reduces mitochondrial function through PGC-1α and several other mitochondrial enzymes.
NAD+ mechanism
NAD+ is a coenzyme that activates enzymes in the body that support REDOX reactions (electron transfer). These enzymes include Sirtuins, polyADP ribose polymerase (PARP), and CD38. These enzymes, which use NAD+, also break down NAD+.
Typically, increased activity of other enzymes that use NAD+ reduces the available NAD+. This reduction in NAD+ levels can inhibit Sirtuins.
Activation of Sirtuin
Sirtuin enzymes turn off certain genes that promote aging, such as those involved in inflammation, fat synthesis and storage, and blood sugar management.
Humans have 7 different Sirtuin enzymes, but in this article we focus on Sirt1 and Sirt3.
Sirtuins are enzymes that use NAD+ to extract acetyl groups (deacetylation) from proteins for modification.
The more NAD+ levels increased, the higher the activity of Sirtuins (niacinamide, on the other hand, blocked the activity of Sirt1).
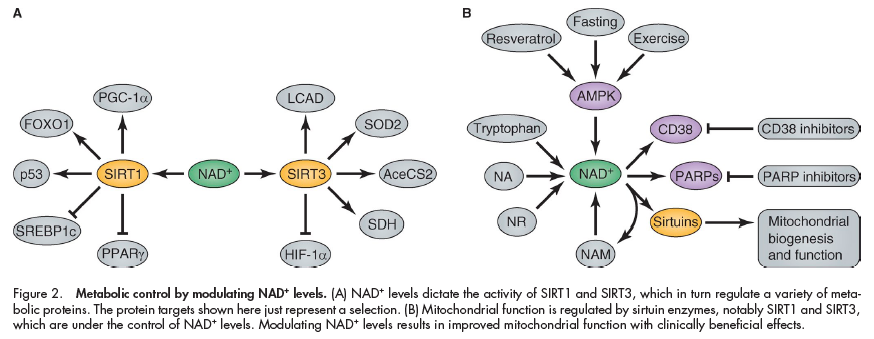
When activated by NAD+, Sirt1 activates:
- PGC-1α stimulates mitochondrial biogenesis and increases fatty acid oxidation
- FOXO1, part of the insulin signaling pathway. FOXO1 activation reduces lipogenesis by inhibiting PPARγ
- p53, a tumor suppressor (anti-cancer) gene, prevents cells with DNA damage from growing into cancer
- SREBP1c, which controls blood sugar, fatty acids, and fat production in response to insulin. It can also control cholesterol levels.
- PPARγ increases insulin sensitivity and insulin secretion. It’s an inflammatory gene.
- Genes that control circadian rhythms
Sirt3, when activated by NAD+, causes these changes in mitochondria:
- Activation of SOD2, a mitochondrial antioxidant enzyme.
- The activation of mitochondrial enzymes responsible for breaking down fatty acids and carbohydrates for energy, including LCAD, SDH, and AceCS2.
- The inactivation of HIF-1α, a protein that is produced when oxygen is deficient.
Activation of PARP, an enzyme that repairs damaged DNA
PARP (PolyADP ribose polymerase) activity requires NAD+. PARP is an enzyme that repairs DNA in response to injury or cellular stress.
PARP activity was associated with maximum lifespan in 13 mammal species. For example, PARP activity in humans is five times higher than in rats. People who live to 100 also have higher PARP activity.
When there is a lot of DNA damage in the cells, inhibition of PARP can lead to apoptosis. Therefore, PARP inhibitors are being tested as anti-cancer therapies.
Mice without PARP had increased NAD+, Sirt1 activity, and experienced some metabolic benefits.
Sum up
Nicotinamide adenine dinucleotide (NAD) is a coenzyme composed of adenine and nicotinamide. It is part of the electron transport chain in mitochondria and is essential for energy production.
NAD+ is sometimes referred to as the “youth molecule” because levels of NAD+ drop dramatically as humans age. Low NAD+ is also associated with hypoxia, skin damage, fatigue, weight gain, metabolic syndrome, cardiovascular disease, and other harmful conditions.
Exercise and diet (caloric restriction) are one of the best ways to increase NAD+, while chronic inflammation, disrupted sleep schedules, and overeating can all reduce NAD+.