[Must see] Efficient liver protection, these drugs you must know! Complete analysis of pharmaceutical care
Clinically, drugs that improve liver function, promote liver cell regeneration and enhance liver detoxification function are classified as hepatoprotective drugs.
There are many reasons for liver cell damage, therefore, in the liver protection treatment, the cause should be removed first, and then the liver protection treatment can be effective.
Liver drugs are usually divided into
- Vitamins and coenzymes;
- Detoxification and liver protection drug;
- Anti-inflammatory and hepatoprotective drugs;
- Essential phospholipids;
- Gallbladder and liver protection drugs;
- Enzyme lowering drugs;
- Drugs for hepatic encephalopathy;
- Other drugs and other eight categories.
The characteristics and key points of pharmaceutical care of commonly used liver protective drugs in clinic were reviewed to provide reference for rational drug use in clinic.
Vitamins and coenzymes
Promote energy metabolism and maintain the normal activity of various enzymes required for metabolism.
It mainly includes various water-soluble vitamins, such as vitamin C, B complex vitamins and coenzyme A.
Fat soluble vitamins may increase the burden on the liver when the dose is large, and it is generally avoided when the liver function is damaged.
Detoxification and liver protection drug
Can provide sulfhydryl or glucuronic acid, enhance the detoxification function.
Including liver Tyrol, glutathione, tiopronin, penicillamine and so on.
1. Reduced glutathione (GSH)
A tripeptide containing active sulfhydryl groups composed of glutamic acid, cysteine and glycine.

Reduced glutathione combines with peroxides and free radicals in the body, fights against the destruction of sulfhydryl by oxidants, protects the proteins and enzymes containing sulfhydryl in cells, and fights against the damage to organs.
Indications:
(1) Liver diseases: including liver damage caused by viruses, drugs, alcohol and other chemicals.
At present, more studies are focused on the protective effect of GSH on alcoholic liver disease and liver fibrosis. The “second strike” theory of the pathogenesis of non-alcoholic fatty liver believes that oxygen stress and lipid peroxidation are the basic mechanisms of fatty liver and liver fibrosis.
GSH can remove free radical antioxidants by binding sulfhydryl groups to free radicals in the body.
(2) Tumor chemotherapy: especially high-dose chemotherapy, can reduce the side effects of chemotherapy, and has no significant impact on the effect of chemotherapy.
(3) Radiotherapy: It can reduce the tissue damage caused by free radicals generated by radiation, especially the diarrhea caused by digestive tract damage.
Common dose:
- Viral hepatitis: 1.2g, qd, 30 days;
- Active cirrhosis: 1.2g, qd, 30 days;
- Severe hepatitis: 1.2-2.4g, qd, 30 days;
- Fatty liver: 1.8g, qd, 30 days;
- Alcoholic hepatitis: 1.8g, qd, 14-30 days;
- Drug-induced hepatitis: 1.2-1.8g, qd, 14-30 days.
2. Tiopronin
Provides sulfhydryl, detoxification, antihistamine, scavenging free radicals and protecting liver cells.
Tioprene prevents peripheral leukopenia and secondary tumor induced by chemoradiotherapy.
It can improve the liver function of acute and chronic hepatitis, and can also be used for the treatment of fatty liver, alcoholic liver, drug-induced liver injury and detoxification of heavy metals.
Oral absorption is easy, liver metabolism, most of it is excreted by urine.
Adverse reactions: Similar to penicillamine, it may cause all the adverse reactions that penicillamine has, but the incidence is lower than penicillamine.
Mainly include
- Agranulocytosis, thrombocytopenia;
- Abnormal taste, nausea, vomiting, abdominal pain, diarrhea, etc.
- Proteinuria (10%), urine discoloration; Pneumonia, pulmonary hemorrhage, bronchospasm, etc.
- Rash, pruritus, urticaria and muscle weakness.
3. Penicillamine
It can complex heavy metals to form a stable water-soluble substance that is excreted by urine and used for copper deposition in tissues caused by heavy metal poisoning and hepatolenticular degeneration.
Adverse reactions: may occur after use
- Allergies;
- Digestive tract reaction;
- Abnormal taste;
- Proteinuria;
- Granulocytopenia and other adverse reactions.
Contraindications: allergy; Severe liver disease and kidney disease; Pregnant and nursing women; Contraindicated in patients with systemic lupus erythematosus.
Usage: 500 to 1000mg daily, divided doses.
Anti-inflammatory and hepatoprotective drugs
It is mainly glycyrrhizin preparation and has adrenocorticoid-like effect without obvious corticosteroid like side effects.
Promote bile pigment metabolism, reduce ALT and AST release, have yellowing and detoxification effects;
Inhibit the formation of free radicals and lipid peroxidation, protect liver cells and anti-fibrosis;
Inhibiting the release of histamine from mast cells has anti-allergic effect;
Inhibit the formation of cell membrane phosphatase A2 and prostaglandin E2, and have anti-inflammatory effects.
Common adverse reactions:
Adrenal corticosteroid side effects were the most common adverse reactions of glycyrrhizic acid drugs, accounting for about 78%. The main clinical manifestations were water and sodium retention or hypokalemia, hypertension, pseudoaldosteronism, diabetes insipidus, breast development and lactation.
Among them, water and sodium retention and hypokalemia are more common, accounting for more than 50%.
1. Diammonium glycyrrhizinate
The third generation extracts of active ingredients of Glycyrrhiza have strong anti-inflammation, protection of liver cell membrane and improvement of liver function in a dose-dependent manner.
Indications:
It is mainly used for chronic persistent hepatitis and chronic active hepatitis with elevated alanine aminotransferase.
Usage:
Orally, 150mg, tid; Intravenous drip, 150mg, qd.
During treatment, blood pressure, serum potassium and sodium concentrations should be monitored regularly. If hypertension, sodium retention and hypokalemia occur, the drug should be reduced or discontinued.
2. Compound glycyrrhizin
The tablets are composed of glycyrrhizin, glycine and methionine. Glycine and methionine can inhibit the decrease of urine volume and sodium excretion caused by glycyrrhizin.
The injection is composed of glycyrrhizin, glycine and cysteine hydrochloride.
Glycine and cysteine hydrochloride can inhibit or alleviate pseudoaldosteronism caused by electrolyte metabolism disorder caused by long-term heavy use of glycyrrhizin.
It has the effects of anti-inflammation, immune regulation, inhibiting liver cell damage and inhibiting virus proliferation.
Indications:
It is clinically used to treat chronic liver disease and improve abnormal liver function.
Usage:
Oral, 2-3 tablets, tid; Intravenous or drip: 40-60 mL, qd, maximum dose 100ml.
Main adverse reactions:
Cardiovascular system: Shock may occur; Metabolic/endocrine system: headache, fever, paresthesia, pseudoaldosteronism, manifested by low potassium, hypertension, water and sodium retention, edema, etc. Musculoskeletal system: rhabdomyolysis, manifested by decreased muscle strength, etc. Allergic reactions: rashes, etc.
Contraindications:
Contraindicated in patients with aldosterone, myopathy, hypokalemia, and advanced cirrhosis with elevated ammonia (methionine metabolites inhibit urea synthesis and reduce ammonia elimination).
3. Magnesium isoglycyrrhizinate
Glycyrrhizic acid is a single trans-optical isomer, a hepatocellular protective agent, with anti-inflammatory, hepatocellular protection, anti-biological oxidation and anti-apoptosis pharmacological effects.
Indications:
It is clinically used for chronic viral hepatitis to improve abnormal liver function.
Usage:
0.1g was diluted with 250ml 10% glucose injection and then injected intravenously, qd, 4 weeks for 1 course.
Essential phospholipids
Phospholipids are the basic components of human cell and tissue membrane system, and play an important role in membrane dependent metabolism, cell regeneration and detoxification.
Liver disease usually involves damage to liver parenchymal cells and organelles, accompanied by loss of phospholipids.
Essential phospholipids can play an important role in liver cell regeneration and remodeling by supplementing exogenous phospholipids and binding to the structure of liver cell membrane.
It can also be secreted into bile, improve the proportion of cholesterol and essential phospholipids in bile, increase the water solubility of bile components, and reduce the gallstone formation index.
Polyene phosphatidylcholine
Indications: various types of liver disease,
- Hepatitis, liver necrosis, liver coma, fatty liver;
- Bile obstruction;
- Poisoning;
- Prevent recurrence of gallstones;
- Treatment before and after surgery, especially hepatobiliary surgery;
- Poisoning of pregnancy, including vomiting;
- Psoriasis, neurodermatitis, radiation syndrome, etc.
Usage:
Orally, starting at 456mg, tid, maximum daily dose is 1368mg, maintenance dose is 228mg, tid; Intravenous infusion: 228-456mg, qd, maximum daily dose is 1860mg.
Gallbladder and liver medicine
1. Adenosylmethionine butyldisulfonate
Adenosylmethionine is a biologically active molecule present in all tissues and body fluids of the human body and involved in important biochemical reactions as a precursor to methyl donors.
A normal concentration of adenosylmethionine in the liver helps prevent intrahepatic cholestasis.
Indications:
It is used to treat intrahepatic cholestasis before and after cirrhosis, intrahepatic cholestasis during pregnancy.
Usage:
The initial treatment is powder injection, 0.5-1g daily intramuscular or intravenous injection for the first 2 weeks; Maintenance treatment was enteric-coated tablets, 1-2g orally per day.
It should be taken orally as a whole tablet, and intravenous medication should not be compatible with alkaline, calcium-containing or high-permeable fluids.
2. Ursodeoxycholic acid
The isomer of normal bile components can promote the secretion of endogenous bile acids and reduce reabsorption.
Antagonize the cytotoxic effect of hydrophobic bile acids and protect liver cell membrane;
Inhibit liver cholesterol synthesis, dissolve cholesterol stones, and have immunomodulatory effects.
Indications:
Cholesterol gallstones, primary cholestatic cirrhosis, primary sclerosing cholangitis and bile reflux gastritis.
Dosage: 10-15mg/kg/d.
Enzyme lowering drug
The intermediate of synthesis of schisandra propyl has obvious induction effect on cytochrome P450 enzyme activity, so as to enhance the detoxification ability of carbon tetrachloride and some carcinogens.
Common varieties are biphenyl diester and bicyclic alcohol tablets, both of which have similar structures, are metabolized by the liver, and most of them are excreted by feces.
1. Biphenyl diester
It has the advantages of rapid enzyme reduction, convenient application and low price. Disadvantages: easy to rebound after stopping the drug.
It is mainly seen in patients with chronic hepatitis, especially in patients with chronic active hepatitis where hepatitis B virus DNA is in a highly replicating state.
Indications:
It is used to improve the main symptoms of persistent hepatitis, such as liver pain, weakness, abdominal distension, and long-term single alanine aminotransferase abnormalities.
Administration: Oral, 7.5-15mg, tid.
The curative effect of treatment of viral hepatitis is related to the patient’s condition, the curative effect of acute hepatitis is the best, followed by mild chronic hepatitis, and it is ineffective for patients with moderate chronic hepatitis and cirrhosis, and even can aggravate liver damage.
2. bicyclol
The structure is similar to that of biphenyl diester. It is used to treat elevated aminotransferase caused by chronic hepatitis.
Administration: Oral, 25-50mg, tid.
The course of treatment should be at least 6 months or as directed by the doctor, and the dosage should be gradually reduced.
Patients with decompensated cirrhosis, such as significantly elevated bilirubin, hypoproteinemia, cirrhosis ascites, esophageal variceal bleeding, hepatic encephalopathy and hepatorenal syndrome should be treated with caution.
Medication for hepatic encephalopathy
1. Ornithine aspartate
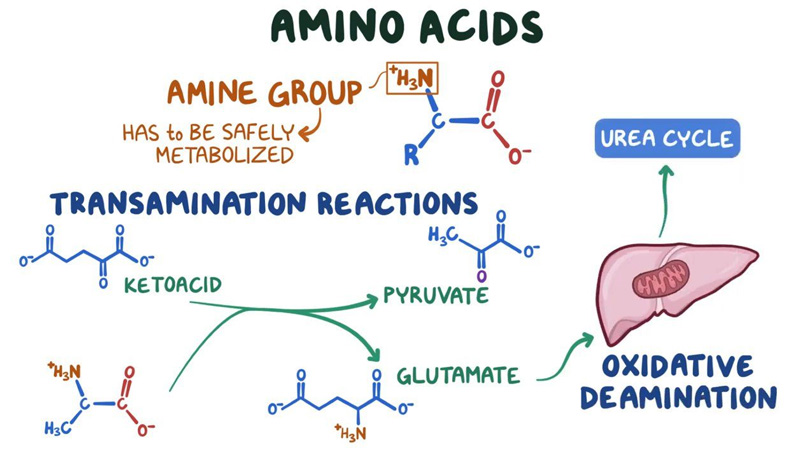
Directly involved in liver cell metabolism, so that most of the blood ammonia ingested by liver cells is combined with ornithine, and metabolized through the urea cycle to produce urea, and finally excreted in a non-toxic form;
Provide intermediate products of energy metabolism, enhance liver energy supply and liver detoxification function.
Indications:
For acute and chronic liver disease caused by elevated blood ammonia and hepatic encephalopathy.
Usage:
Oral, 5g, bid; Intravenous infusion, 5-10g/d for acute hepatitis, 10-20g/d for chronic hepatitis or cirrhosis, maximum dose 40g/d.
2. arginine
Important amino acids in the body, involved in the ornithine cycle, promote urea synthesis in the body and reduce blood ammonia, improve symptoms.
Indications: It is used for mental symptoms caused by excessive blood ammonia for various reasons.
Administration: Intravenous infusion, 10-20g, qd. Blood gas analysis should be monitored during medication.
Contraindications: renal insufficiency is prohibited.
3. Branched chain amino acid
The imbalance of serum amino acid balance, especially the decrease of branchchain amino acid and the increase of aromatic amino acid, is easy to occur in cirrhosis and liver dysfunction.
By increasing the concentration of serum branchchain amino acids, the imbalance of the two kinds of amino acids was reversed and the function of central nervous system was restored.
Usage: 250ml, bid.
Rapid infusion may result in nausea, vomiting, headache, fever, etc.
Other drugs
1. Potassium magnesium aspartate
It is a precursor of oxaloacetic acid in the body and plays an important role in the tricarboxylic acid cycle, but also participates in the ornithine cycle and promotes the metabolism of ammonia and carbon dioxide.
Indications: acute jaundice hepatitis, liver cell dysfunction, can also be used for other acute and chronic liver diseases.
Usage: 10-20ml, add 5% or 10% glucose injection 250-500ml slowly intravenous drip.
2. Silybin silybin
A flavonoid derived from the fruit of the milk thistle of the genus thistle in the chrysanthemum family.
Indications: For the treatment of chronic persistent hepatitis, chronic active hepatitis, incipient cirrhosis, liver poisoning and other diseases.
Administration: Oral, 2 tablets, tid.
Adverse reactions: nausea, hiccup, chest tightness, etc. Use with caution for pregnant and lactating women, the elderly and children.
When treating fatty liver and cirrhosis, it is not appropriate to use too much high-fat food.
3. Oleanolic acid
It was put forward by the Chinese herbal medicine factory and can also be extracted from the pharmaceutical residues of fructus ligustris syrupus.
It can significantly reduce the serum alanine aminotransferase of experimental liver injury animals, alleviate the degeneration and necrosis of liver cells and the inflammatory reaction and fibrosis process of liver tissue, and promote the regeneration of liver cells.
Indications: For viral migratory chronic hepatitis.
Administration: Oral, acute jaundice hepatitis 30mg, tid; Chronic hepatitis 50mg, qid.
4. matrine
Alkaloids extracted from matrine can prevent liver fibrosis, prevent liver cell apoptosis, stabilize cell membrane, remove free radicals, protect liver cells and regulate immunity.
Indications:For the treatment of chronic viral hepatitis B.
Usage: Oral, 0.2-0.3g, bid; Intramuscular injection, 0.4-0.6g, qd; Intravenous drip, 0.6g, qd.
5. Hepatocyte growth promoting hormone
The small molecular weight polypeptides extracted from the fresh liver of Suckling pig can stimulate the DNA synthesis of normal liver cells and promote the regeneration of liver cells.
Indications: Mainly used for the adjuvant treatment of subacute severe hepatitis (viral, early or middle stage of liver failure).
Administration: intramuscular injection, 40mg, bid; It can also be added 80-120mg to 10% glucose injection intravenous drip, qd, a course of 8-12 weeks.